Recently the ruling Congress-NCP government in Maharashtra decided to accord 16% reservation for Marathas and 5% for Muslims in government jobs and educational institutions in a last-ditch attempt to woo these two categories of people following the parties’ pathetic performance in Lok Sabha elections. This again raises the same question which we have been choosing to ignore until now, when will this spiraling trend of increasing proportion of caste based reservations end?

Coming from a very moderate background, I have managed to achieve a lot in the prevailing adversity of the Indian caste based reservation system. Until now I have not complained but there has to be a point where you have to say ‘enough is enough’.These type of politically motivated actions are really demotivating and it makes me feel that our coming generation will really have to struggle hard to get quality education and rightful opportunities, if such actions don’t face a strong opposition right now. I am sure that majority of people reading this blog will also resonate with my concerns.

The whole logic of caste based reservations is wrong at so many levels. Below I discuss a few reasons why a caste based reservation system is out rightly illogical and should be discarded.
1. The term ‘backward classes’has not been clearly defined anywhere in the constitution.
What actually constitutes a backward class? What are the determinants of a backward class? Since a clear definition is lacking, it is being utilized by politicians to lure vote banks.
2. Caste of a person is just a confounding proxy factor to ascertain the backwardness of an individual.
Instead of a correct identification of actual backward classes, castes system has been conveniently adopted as a proxy without considerations of proper checks to insure the validity of elementary factors like poverty, literacy, occupation and place of habitation.
3. The Indian caste based reservation system assumes the rest of the population belonging ‘General Category’have normal social indicators and no person is backward if he belongs to the so called‘General Category’!
There many economically worse off children belonging to the general category, many of them may be even living below poverty line; even then they cannot get the fruits of such reservation merely by virtue of belonging to the ‘general’ category.
4. Currently there are no timelines for this social intervention!
Once a caste is tagged as backward, for how many years it will continue receiving the preferential status? The roots of the current structure of caste based reservation system can be traced back to the report by the Mandal commission which was established in 1979 by the central government to identify the socially or educationally backward in India and suggest measures for their upliftment. Today, after more than 30 years of the Mandal commission and 60 years of republic India; how many castes have been revoked of their reserved status?
5. These policies have been in India since more than 30 years and they have failed to meet any objectives other than giving edge to some political parties.
The government should go into the reasons of the failure. Many students despite of their reserved status of their caste don’t make it to the institutes, so the real question is, is it actually their caste which is the variable for backwardness even after 50 years of the operational caste based reservation system.
6. There are no monitoring mechanisms to the caste reservation system of India.
Once a caste is tagged as backward, what are the criteria to ascertain that backwardness is being alleviated by reservations? What are the indicators that are being monitored that the true beneficiaries are actually getting the benefits and false beneficiaries are not getting the benefits?
7. No disclosure of influence on social indicators by the government.
Since the caste based reservation system is a preferential distribution of opportunities that the nation is generating, the rest of the public has a right to know the influence on quarterly and annual basis. But there are no such mechanisms for reporting and monitoring of caste based reservation system.
8. Instead of genuinely alleviating the social inequalities, reservations programmes have a very clear electoral objectives.
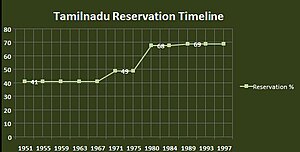
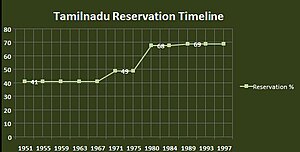
Even a kid who has taken his first lesson in Social Sciences at school can understand the real motive behind the whole caste based reservation system in India. That is why almost always we hear the new castes being included in the reservation pool just before the elections, how coincidental is that? Currently 49.5% of the seats in premier institutions are reserved for backward categories. This is more than 60 % in some states like Tamil Nadu and now Maharashtra is heading towards 73% after the decision by the ruling Congress-NCP government to give 16% reservation to Marathas (Not a minority, Not backward) and 5% reservations for Muslims (Religion based reservation, Unconstitutional)!

9. There is a complete skewing of the distribution of seats and opportunities in the population towards a few preferential reserved castes.
A reserved candidate can opt for both an open seat and a reserved seat. In a case if both seats are available to the reserved candidate, open seat is allotted first. On the other hand an unreserved candidate can only opt for an open seat. But since many of these have already been allotted to meritorious reserved candidates, they are not available for open category candidates. In some states which are providing up to 70% reservations, the proportion of candidates from reserved castes in the opportunity pool reaches up to 95% (including the meritorious students in the reserved castes), completely neglecting the representation of rest of the population creating a sort of caste based oligopoly.
10. By current policies it is even justified for the creamy layers to take the benefits meant to alleviate the backwardness!
This ‘creamy layer’ policy excluded the creamy layer (people with income above a certain range) only among the OBCs, not among the SCs and STs. This creamy layer policy has only been implemented in some states.


11. Some individuals consider this as the reversal of the oppression their ancestors have faced.
There are two flaws in this logic. Firstly, the current social system has changed drastically as compared to its state decades ago, the hypothesis that certain classes are still facing oppression in terms of opportunities to grow is false in my view and should be retested. Secondly, there are many classes and sects which were not a part of the Indian caste system who have migrated to India due to partition or otherwise; are not they facing a sort of reverse oppression in the current scenario? They were neither a part of this so called historical oppression nor were they given any preferential opportunities but have managed to sustain, rising from scratch after partition.

The stance I have adopted is very clear, equality and equity is right of every individual in this country. By their very definition, the promotion of equality and equity are virtues which cannot be retrospectively applied but have to be strongly rooted in the present. In the current form the caste based reservation system may benefit a few individuals but there would be a great number of individuals who will enjoy the benefits without needing them. While there will be a set of individuals who are actually in need but are not from the reserved categories who would fail to receive any benefit. Instead of eliminating the caste based divisions, this mechanism is actually strengthening the existence of caste delineation in our society.


It will be very difficult to do away with this spiraling increase in the reservations term after term, since no party would out rightly deny the support to such a decision or oppose it in the fear of losing the vote bank. The ruling parties in many instances have even defied the Supreme Court judgement capping quotas at 50% by making amendments to the state laws. . Only solution I can think of is challenging such illogical decisions in Supreme Court or speak the language what the political outfits understand- the language of Votes! We should all take a note of parties and entities promoting and giving off reservations and take an informed decision while at the ballot to vote them out of power!
References
- http://timesofindia.indiatimes.com/home/opinion/edit-page/Reservation-for-Marathas-and-Muslims-in-Maharashtra-might-backfire-on-Congress-NCP/articleshow/37268930.cms
- http://www.youthkiawaaz.com/2010/02/our-fate-in-the-hands-of-reservations/
- http://www.youthkiawaaz.com/2011/02/educational-reservations-india-solutions/
- http://en.wikipedia.org/wiki/Creamy_layer
- http://en.wikipedia.org/wiki/Reservation_in_India